About a year ago, CMS approved reimbursements for low-dose CT (LDCT) for lung cancer in Medicare patients (provided the patient meets certain criteria). This was big news because it is the first time that Medicare paid for lung cancer screening, and because lung cancer is a leading cause of cancer deaths in the U.S. Medicare coverage includes a visit for counseling and shared decision-making on the benefits and risks of lung cancer screening. With pulmonologists and imaging centers gearing up to provide these screenings, a mixed bag of opinions and perceptions are emerging. As uncertainty and misperceptions abound, one thing is clear: more education is needed by physicians and patients alike to ensure that LDCT can provide the intended results.
Screening Criteria
To qualify for annual Medicare reimbursement for LDCT, patients must meet ALL of the following criteria:
- Be age 55-77 and either current smokers or former smokers (within the last 15 years).
- Have a tobacco smoking history of at least 30 “pack years” (an average of one pack a day for 30 years).
- Receive a written order from a physician or qualified non-physician practitioner that meets certain requirements.
Different Low-Dose CT Lung Cancer Screening Studies
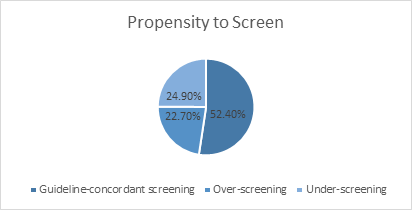
It’s interesting to see the how doctors and patients see the value of LDCT lung cancer screening. We looked at results of two different studies to see if pulmonologists would over-screen, under-screen or screen according to guidelines, as well as how the screening may affect smokers.
Pulmonologists
Jonathan M. Iaccarino and associates conducted a nationwide web-based survey among active staff pulmonologists in Veterans Health Administration pulmonary clinics from July 2013 to February 2014 to gauge their likelihood of conducting annual LDCT screening for qualified patients. Out of 574 eligible pulmonologists emailed, 286 (49.8%) participated. Roughly half of the respondents said they would use the screenings according to guidelines, and the other half would either over-screen or under-screen (with that group split almost in half).
As a result, Iaccarino and associates concluded that “pulmonologists have varied perceptions of the evidence and trade-offs of LDCT screening, leading to potential for over- and under-screening. To minimize potential harms as LDCT screening is widely implemented, physicians must understand which patients are appropriate candidates and engage patients in a shared decision-making process regarding the trade-offs of LDCT screening.”
286 Pulmonologists and their propensity to use annual LDCT screenings for lung cancer
Data from: http://www.atsjournals.org/doi/abs/10.1513/AnnalsATS.201507-467OC#.Vik-EGtrVqp.
Smokers and Low-Dose CT Lung Cancer Screening
Steven B. Zeliadt, PhD, MPH and several colleagues conducted a study of 37 individuals from June 15, 2014 to March 29, 2015. The study included telephone interviews to current smokers. The results show that screenings did prompt most of the current smokers to reflect on the health ramifications of smoking for the first time. However, he notes that “17 of 35 (49%) participants described mechanisms whereby screening lowered their motivation for cessation, including the perception that undergoing an imaging test yields the same health benefits as smoking cessation.”
Misperceptions about the benefits of LDCT lung cancer screening
Quoted directly from Zeliadt’s published results, other misperceptions that could lead to serious ramifications include:
- The belief that everyone who participates in screening will benefit.
- The belief that screening and being able to return for additional screening offers protection from lung cancer.
- The perception by some individuals that findings from screenings have saved their lives by catching their cancer early when indeterminate findings are identified that can be monitored rather than immediately treated.
- A reinforced belief in some individuals that a cancer-free screening test result indicates that they are among the lucky ones who will avoid the harms of smoking.
Is screening a positive or negative?
Both. Obviously, catching cancer early is a positive. Some people, however, think that the screening is a substitute for quitting smoking. Not only is that false information, it’s a dangerous misconception.
In addition, some screenings can show false positive results. Abnormal findings may require additional testing to determine whether or not cancer is present. These tests, such as additional CT exams or more invasive tests such as biopsy, have risks and may cause a patient anxiety.
Ultimately, the level to which a healthcare provider sees the benefits of LDCT screening will affect whether he or she orders the tests. And how the results are explained will make the difference in how a patient interprets the need to quit smoking.
Final Thoughts | Low-Dose CT Lung Cancer Screening
With any screening, it is important to have the exam done on quality equipment at an accredited facility. RadSite can help you evaluate your CT imaging systems and certify they are operating at the optimal level of performance, so you can provide quality care for your patients.

